Global health consultant & author
Turning evidence into action
for sustainable health impact
Welcome!
At Health System Metrics, we partner with governments, civil society, and global agencies to turn robust evidence into practical solutions that deliver measurable, sustainable health impact. With a proven record in complex environments across Asia, the Pacific, and Africa, we combine technical leadership, advanced analytics, and deep regional expertise to design and implement integrated, resilient health systems that achieve lasting improvements.
Our approach
We translate global best practice and robust data into tailored, context-specific solutions—ensuring every intervention leads to measurable, lasting change.
- Collaborative and capacity-building: We work side-by-side with you to build skills, ownership, and sustainable results.
- Equity and rights-focused: We embed human rights and inclusion at every step, with a focus on key and vulnerable populations.
- Disease-specific expertise: Deep experience in HIV, TB, malaria, maternal and child health, and pandemic preparedness.
What we do
We provide technical support, strategic advice, and hands-on implementation to help clients achieve resilient, high-performing health systems. Our core services include:
- Health Systems Strengthening
Analysis, design, and implementation of integrated, resilient health system reforms. System gap analysis, strategic planning, and policy alignment.
- Program Design and Evaluation
Mixed-method evaluations (quantitative and qualitative), advanced analytics, and learning-focused reviews. Application of international frameworks (OECD/DAC, traffic-light, WHO standards).
- Strategic and Technical Advisory
Organisational development, technical leadership, and high-level policy advice. Implementation science and capacity building for government and NGO partners.
- Human Resources for Health
Workforce planning, HRH strategy development, retention and regulatory systems. Digital HRH data systems and evaluation frameworks aligned with WHO and OECD-DAC standards.
- Health Financing and Cost Analysis
Investment case development, deep cost analysis, financial modelling, and innovative financing (e.g., social contracting). Fiscal space analysis and sustainability planning.
- Digital Health and Data Systems
Digital health system assessments, data governance, and interoperability. Development of data-sharing protocols and real-time dashboards.
- Consensus-Building and Facilitation
Delphi workshops and participatory methods to align diverse stakeholders. Multi-stakeholder engagement, workshop facilitation, and risk management.
- Community Health Systems
Community-based service delivery, participatory planning, local capacity building, and integration of community health workers. - Rights-Based and Equity Approaches
Integration of gender equity, human rights, and inclusion into program design and delivery. Addressing legal and structural barriers to access for key and vulnerable populations.
Our approach is hands-on and adaptable, ensuring strategies are practical, evidence-based, and sustainable—whether for epidemic response, system reform, or resource mobilisation.
Learn more about our leadership and achievements →
Testimonials
“Jim Rock’s leadership was pivotal in building East Timor’s first national HIV program-his technical expertise and collaborative approach delivered real results.”
- Dr. Charles Oliver, Country Director (a/g), USAID Timor-Leste
“As RSSH Focal Point on the Technical Review Panel, Jim Rock co-led a team of experts to review USD 12 billion in investments, and played a key role in the pivotal 2021 advisory review that guided the Global Fund’s future investments in resilient health systems…”
- Dr. xxx, Chair, Global Fund Technical Support Facility
Lets work together!
Whether you need a strategic advisor, technical partner, or hands-on implementer, Health System Metrics is ready to help you achieve your goals.
Contact us to discuss your needs and explore how we can collaborate for stronger, more sustainable health systems.
Contact
Health System Metrics
Jim Rock, Principal Consultant
📩 jtarock@gmail.com
📞 +61-404447850
Or get in touch via LinkedIn:
https://www.linkedin.com/in/jim-rock-hsm/
References and detailed project portfolio available upon request.

Real world results
Health System Metrics has delivered results for governments and partners, including:
- Securing major funding for integrated HIV, TB, and health system programs
- Designing and implementing national health workforce strategies
- Building digital data systems for real-time decision-making
- Supporting Global Fund, PEPFAR, and USAID grant implementation
- Developing and scaling communicable disease and primary health care programs
1. National HIV Program Design and Scaleup – Timor-Leste

Tip: Click anywhere on the section below to expand and read more.
Led the country’s first national HIV/AIDS program, building local capacity, generating the first HIV/STI data, and securing major Global Fund investment.
- Evidence-Based Program Design: Conducted the country’s first behavioural and biomedical surveys to inform targeted prevention and care for high-risk groups.
- Capacity Building: Trained 250+ clinic staff and 389 peer educators, including police, military, and community members.
- Service Delivery: Established VCT and STI services, reaching 145+ for HIV testing and 65 for STI care; initiated ART for the first 10 patients.
- Prevention Impact: Distributed 260,000+ condoms and developed national behaviour change communication strategies.
- Policy and Funding: Supported the Ministry of Health in developing the first National HIV/AIDS Strategic Plan and secured major Global Fund investment for scale-up.
- Recognition: Program recognised for technical and management excellence by the Minister of Health and USAID.
For further details, see the full final report (PDF).
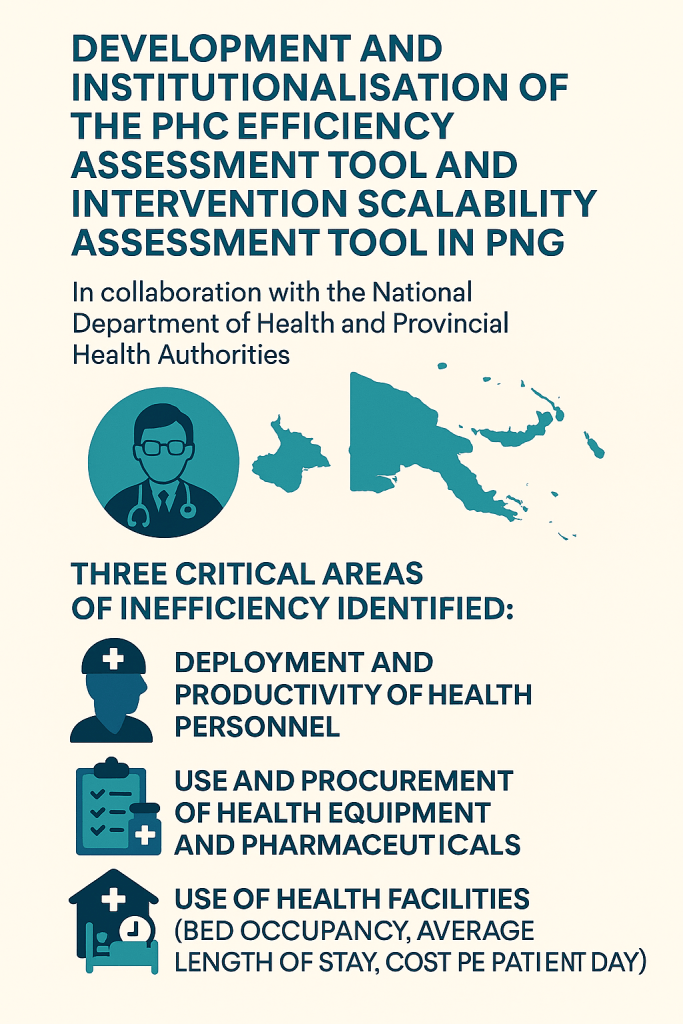
2. Efficiency in Papua New Guinea’s health system

Tip: Click anywhere on each section below to expand and read more.
Designed and institutionalised analytical tools to improve PHC efficiency, leading to measurable service delivery gains and more effective resource allocation
- Developed and rolled out a PHC efficiency assessment tool, now used for budgeting and policy at facility and national levels
- Prepared the 2020 HIV Investment Case, demonstrating that full strategy implementation would avert 15,000+ new infections and save $13M by 2022.
- Delivered a 20-year Global Fund investment review, guiding future strategy and highlighting the need for integration and sustainability.
3. Global Fund support
Shaped global investment frameworks and improved performance measurement for resilient health systems
- As RSSH Focal Point in the Technical Review Panel, advised on technical quality and strategic merit of $12B+ in grant proposals (2017–21).
- Co-led the TRP’s 2021 “deep dive” and report that shaped the Global Fund Board’s RSSH investment framework.
- As OIG consultant, identified gaps in RSSH and pandemic preparedness investment monitoring and recommended improvements in performance measurement and risk management.
4. Sustainability -Asia
Tip: Click anywhere on the section below to expand and read more.
Coordinated baseline assessments in four countries, strengthening financial sustainability, strategic information, and community engagement for HIV services.
- Led rapid baseline assessments in Bhutan, Mongolia, the Philippines, and Sri Lanka.
- Identified gaps and opportunities in financial sustainability, strategic information, programmatic sustainability, and human rights.
- Recommendations included formalising social contracting, integrating community-led monitoring, scaling up innovative service models, and enhancing legal protections
- Led team of 12 international and national experts
5. Procurement and Systems Reform – Afghanistan

Supported transparent, World Bank-compliant procurement for a $600M health project, improving accountability and contract management.
- Guided the Ministry of Public Health in fair contracting for essential services in 31 provinces.
- Developed risk analysis tools and process recommendations to strengthen procurement and accountability.
Insights & Solutions
Explore our latest thinking on integration, HRH, sustainable financing, and rights-based approaches-practical ideas you can apply today.
Why Integration is the Future of Primary Health Care in LMICs

Integrated PHC models deliver measurable gains in efficiency, quality, and equity—here’s how:
Financial Efficiency
- Reduced duplication: Coordinating care across services (like HIV, TB, and maternal health) minimises unnecessary tests and procedures, lowering costs for patients and health systems.
- Preventive savings: Focusing on prevention through PHC, such as immunisations and chronic disease management, reduces the need for expensive hospital care.
- Optimised workforce: Cross-trained community health workers and nurses deliver a broader range of services, making better use of available staff.
- Equitable financing: Integrated funding models help reduce out-of-pocket expenses, making care more accessible.
Quality Improvements
- Holistic care: Addresses physical, mental, and social health needs together.
- Accountability: Digital tools and community-led monitoring reduce stockouts and improve responsiveness
- Continuity and trust: Ongoing provider relationships improve adherence and satisfaction
Looking Ahead
Countries adopting integrated PHC are seeing positive results—such as improved surveillance in Malawi and increased TB/HIV case detection in Zimbabwe. Integration is a practical path toward universal health coverage and more resilient systems.
In summary, integrated PHC makes health systems more efficient, equitable, and responsive to community needs.
Unlocking fiscal space and making every health dollar count
Tip: Click anywhere on the section below to expand and read more.
WHO estimates up to 40% of health spending is wasted. Our experience in Papua New Guinea and other settings shows how targeted efficiency gains and smarter procurement can unlock substantial resources for frontline health services—even as donor support declines.
- Context and approach
Drawing on the WHO estimate that up to 40% of global health spending is lost to inefficiency, we have seen in Papua New Guinea and other settings how targeted efficiency gains and smarter procurement can identify opportunities to redirect resources to frontline health services.
In Papua New Guinea, Jim led the development and piloting of the Primary Health Care (PHC) Efficiency Assessment Tool and the Intervention Scalability Assessment Tool under the PATH program. These Excel-based tools, designed in collaboration with the National Department of Health and Provincial Health Authorities, systematically identify inefficiencies in:- Deployment and productivity of health personnel
- Use and procurement of health equipment and pharmaceuticals
- Use of health facilities (bed occupancy, average length of stay, cost per patient day
- How the Tools Work
Facility managers and provincial leaders were trained to use these tools to pinpoint where resources might be wasted—such as underused staff, procurement of overpriced or expiring medicines, or costly patterns of hospital admissions. For example, the tools highlight when facilities are overstaffed with administrative personnel, underusing expensive equipment, or maintaining too many empty beds, all of which drive up costs without improving patient care.
- Implementation and Lessons Learned
Although the project was discontinued following the initial advisory phase due to a reprogramming of the overall investment, the approach demonstrated how practical, context-driven reforms can identify opportunities to turn wasted spending into new resources for health—even in challenging environments- Building trust with facility managers, adapting tools to different levels of care, and ensuring data quality all required persistence and flexibility
- The experience in PNG illustrates the value of targeted efficiency analysis and procurement review as strategies to help health systems make the most of every available dollar.
- Results Achieved (advised):
- Reallocated staff to better match patient needs
- Switched to generic medicines and improved stock management
- Adjusted bed numbers or referral patterns to reduce unnecessary costs
- Summary:
Through developing and piloting these efficiency and scalability tools, we have shown how practical, evidence-based reforms can help health systems identify and unlock new resources—even when full implementation is not possible.
Building a resilient health workforce: lessons from the field
Click anywhere on the section below to expand and read more.
As HRH lead for the midterm review of the LAO/035 Health and Nutrition Programme, Jim applied a rigorous, mixed-method evaluation to assess and strengthen the health workforce in Laos, supporting the national HRH Strategy 2030.
Analytical Approach
- Designed a comprehensive evaluation plan, including a 10-day field mission across Vientiane and Bokeo, to validate desk review findings and ensure actionable recommendations.
- Used the full suite of OECD/DAC criteria—relevance, coherence, efficiency, effectiveness, sustainability, and impact—to structure the assessment and reporting.
- Introduced a traffic-light framework to categorise 42 HRH interventions by performance and urgency, enabling rapid strategic prioritisation.
Data Collection and Triangulation
- Conduct 28–35 semi-structured interviews with central and provincial health officials, facility managers, scholarship recipients, and development partners.
- Carry out facility walk-throughs to observe EMR use, licensing logs, and staffing boards, directly validating reported data and practices.
- Audit programme datasets (EMR, HPIMS, DHIS2, HRIS, licensing, financial reports) to measure efficiency, retention, and system integration.
- Cross-check findings by comparing interview insights, observations, and quantitative data for robust, evidence-based conclusions.
Key Insights and Results
- Strategic Alignment: All interventions mapped to HRH Strategy 2030 objectives, with strong policy alignment and local ownership (20% provincial co-financing, updated HRH plans).
- Efficiency and Digital Transformation: EMR rollout in 120 facilities saved staff two hours per week; digitalisation and co-financing reduced donor dependency.
- Quality and Equity: 80% female scholarship participation and a 15% reduction in clinical errors; persistent gaps in licensing coverage and rural workforce distribution remain.
- Actionable Recommendations: Establish a technical working group for data integration, develop bonding and career pathway schemes for rural retention, and deploy mobile assessment teams for quality assurance.
Lessons Learned
- The combination of structured planning, advanced data evaluation, and mixed-method triangulation provided a robust evidence base for decision-making.
- Systematic stakeholder engagement and participatory validation workshops ensured recommendations were grounded in real-world realities.
- The traffic-light framework and real-time validation dashboard enabled rapid identification of priorities and responsive programme adaptation
Summary
This evaluation demonstrates how advanced analytical skills, strategic planning, and a rigorous DAC/OECD approach—combined with deep stakeholder engagement and data triangulation—can drive practical, evidence-based improvements in health workforce resilience and system performance in Laos.